Is estrogen dominance the only key hormone affecting endometriosis?
It is often documented that endometriosis is an estrogen dominant issue. But could there be other imbalances that are at play here?
Endometriosis is an estrogen-dominant issue because estrogen fuels the growth of endometrial-like tissue outside the uterus. This happens through a combination of high local estrogen production within the lesions, a resistance to progesterone, and an increased activity of estrogen receptors in the endometriotic tissue. These hormonal imbalances cause the tissue to grow, inflame, and become painful, contributing to the disease's symptoms.
One of the above factors noted is ‘resistance to progesterone’. So even if women address their estrogen dominance through diet, supplements and life style changes, the problem of low progesterone may still exist.
In endometriosis, when endometrial like tissue grows outside the uterine cavity, progesterone and estrogen signalling are disrupted, commonly resulting in progesterone resistance and estrogen dominance.
Below we look at some of the complex mechanisms of estrogen and progesterone and how they affect different functions and other hormones in the body.
Estrogen and Progesterone: The Balance of Female Hormones
- Estrogen is the builder. Progesterone is the balancer.
- Estrogen stimulates tissue growth, ovulation signals, and even mood. It governs fertility, collagen production, and cardiovascular health.
- But without progesterone to ground it, estrogen becomes unregulated — too stimulating, too inflammatory, too dominant.
- It’s not that estrogen is bad — it’s that it’s unopposed.
- Important Note: You can have estrogen dominance even with “normal” progesterone.
- If estrogen is high, poorly detoxed, or recirculating, it can overpower progesterone — even when your levels fall in the “normal” lab range.
- It’s the ratio and balance that matters more than isolated numbers.
- Progesterone is what calms the system. It relaxes smooth muscles (gut, uterus, vessels), stabilizes mood, regulates the immune system, and signals that ovulation was successful.
- It’s the body’s natural anti-anxiety hormone, anti-inflammatory, and diuretic — and most women are deeply deficient.
𝗣𝗵𝘆𝘀𝗶𝗼𝗹𝗼𝗴𝗶𝗰𝗮𝗹𝗹𝘆, 𝗽𝗿𝗼𝗴𝗲𝘀𝘁𝗲𝗿𝗼𝗻𝗲 𝗶𝘀 𝗮 𝘀𝘁𝗲𝗿𝗼𝗶𝗱 𝗵𝗼𝗿𝗺𝗼𝗻𝗲 primarily produced by the corpus luteum after ovulation, and in smaller amounts by the adrenal glands. It is synthesized from pregnenolone, which in turn is made from cholesterol.
Progesterone binds to specific receptors in the brain, uterus, breasts, and immune cells to regulate gene expression, calm neural activity, and control the inflammatory response. Without sufficient progesterone, many body systems — from mood and metabolism to immunity and sleep — become dysregulated.
𝗣𝗿𝗼𝗴𝗲𝘀𝘁𝗲𝗿𝗼𝗻𝗲 𝗮𝗹𝘀𝗼:
• Boosts GABA, the neurotransmitter of calm and sleep.
• Balances blood sugar and insulin.
• Enhances thyroid function by converting T4 → T3.
• Supports bone density, skin elasticity, and cognitive clarity.
• Protects against estrogen-driven cancers by keeping cell growth in check.
When progesterone drops, estrogen’s effects go unchecked — leading to fluid retention, anxiety, heavy periods, and breast tenderness. It’s not that there’s “too much estrogen” — it’s that progesterone isn’t doing its job.
What looks like estrogen dominance is often progesterone crash
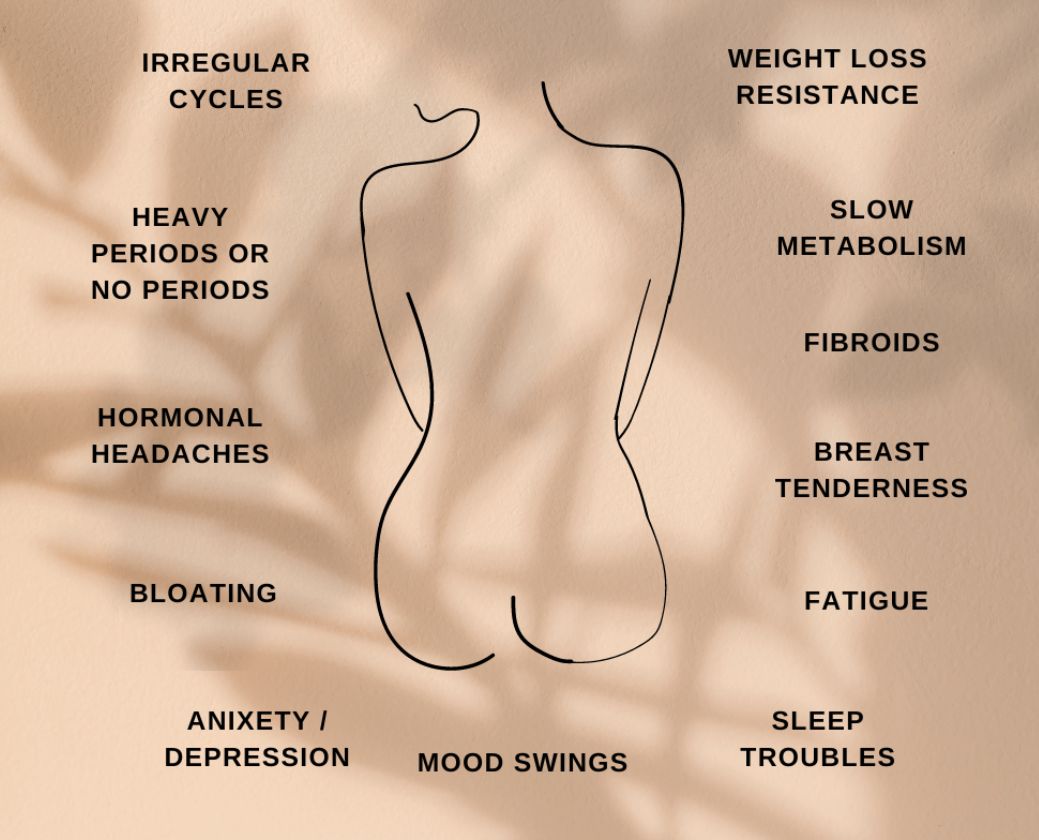
Here are classic symptoms of so-called “estrogen dominance” — all of which can also result from low progesterone
• PMS, mood swings, irritability
• Heavy periods, clotting, cramps
• Breast tenderness, bloating
• Anxiety, insomnia, mid-cycle spotting
• Weight gain around hips and thighs
• Estrogen-sensitive conditions: fibroids, endometriosis, PCOS, and even some breast cancers
You can have normal or even low estrogen — and still feel “estrogen dominant” if there’s not enough progesterone to balance it. Why? Because estrogen amplifies — it excites, grows, and stimulates. Progesterone modulates — it soothes, grounds, and restores.
When that equilibrium shifts, your body speaks loudly through symptoms that get labelled as “hormone imbalance.” But it’s not always an estrogen surplus — it is often a progesterone void.
Why progesterone deficiency is so common
Chronic Stress → Cortisol Steals Pregnenolone
Your body prioritizes survival over fertility. When stressed, pregnenolone (the master hormone) gets diverted to cortisol instead of progesterone — a process known as “pregnenolone steal.” The result? High stress hormones, low reproductive hormones, and a dysregulated nervous system.
Lack of Ovulation = No Corpus Luteum = No Progesterone
Every healthy menstrual cycle should include ovulation. After ovulation, the follicle transforms into the corpus luteum, which produces progesterone for about two weeks. No ovulation means no corpus luteum — and virtually no progesterone. Even “normal” cycles can be anovulatory (no ovulation) due to stress, under-eating, over-exercising, thyroid dysfunction, or blood sugar instability.
Perimenopause → Estrogen Dominates by Default
During perimenopause (late 30s–50s), ovulation becomes irregular, so progesterone plummets years before estrogen does. This leaves estrogen relatively unchecked — causing hot flashes, mood swings, insomnia, and heavier bleeding even while labs may show “normal” estrogen.
Environmental Toxins & Xenoestrogens
Plastics (BPA, phthalates), pesticides, synthetic fragrances, and personal-care chemicals mimic estrogen and overwhelm receptors — tricking the body into thinking there’s plenty of estrogen while blocking progesterone’s effects.
Low Cholesterol or Under-Eating
Hormones are made from fats — specifically cholesterol. Low-fat diets, fasting, and calorie restriction starve hormone production. Without enough building blocks, your body simply can’t make progesterone.
Thyroid Dysfunction
Low thyroid function (even subclinical) reduces luteinizing hormone (LH), which is required for ovulation. It also slows cholesterol conversion into pregnenolone — the first step in progesterone synthesis.
Birth Control Pills
Oral contraceptives shut down ovulation — meaning no natural progesterone production.
Synthetic “progestins” are not the same molecule and do not activate the same calming, anti-inflammatory, or neuroprotective receptors as real progesterone.
Nutrient Deficiencies
Low zinc, magnesium, vitamin B6, selenium, and vitamin E directly impair luteal-phase hormone synthesis.
What happens when progesterone stays low
• Estrogen becomes pro-inflammatory — causing water retention, histamine release, and mast cell activation.
• Insulin resistance and cortisol rise.
• Sleep becomes fragmented due to low GABA and melatonin synthesis.
• Immune balance shifts toward autoimmunity and allergies.
• Brain fog, depression, and anxiety increase as serotonin and dopamine signalling falter.
• PMS and PMDD worsen — not because of “too much estrogen,” but because your brain has lost its progesterone buffer.
Rebalancing progesterone naturally
Rebuild progesterone from the inside out — not by “tricking” the body, but by restoring what it needs to make this hormone on its own.
1. Prioritise ovulation - the main natural source of progesterone
Progesterone is primarily made after ovulation. No ovulation = no corpus luteum = no progesterone. Small amounts are also made in the adrenal glands.
To support healthy ovulation:
• Eat enough calories and carbs (extreme low-carb or undereating shuts ovulation down)
• Address PCOS or insulin resistance if present
• Get morning sunlight to anchor circadian rhythm (key for luteinizing hormone production)
Support thyroid health (check TSH, Free T3, Free T4)
• Avoid seed oils and processed foods that damage the hormonal rhythm
Track your cycle: ovulation may not happen mid-cycle. Use basal body temperature, cervical mucus, or LH strips to confirm ovulation is actually occurring.
2. Calm the nervous system - Cortisol blocks progesterone
High stress = pregnenolone steal = low progesterone.
Rewire your stress response:
• Practice deep belly breathing, vagal toning, or yoga
• Use adaptogens like ashwagandha, rhodiola, or holy basil – these all reduce cortisol but note ashwagandha should not be take by those with auto-immune diseases as it can trigger flares
• Get daily nature time, grounding, or sunlight to lower cortisol
• Sleep before 10PM to preserve circadian hormone rhythm
• Try magnesium glycinate (400–600 mg/day) for GABA support and cortisol control
3. Eat enough healthy fats & nutrients - hormones are built from them
• Egg yolks, grass-fed butter, ghee
• Extra virgin olive oil, coconut oil, avocados
• Fatty fish (wild salmon, sardines) for omega-3s
• Beef liver (rich in vitamin A, copper, B6, and zinc)
Key nutrients for progesterone:
• Zinc – boosts follicle development and ovulation
→ Oysters, pumpkin seeds, grass-fed meats
• Vitamin B6 (P5P) – critical for luteal phase hormone production
→ Pastured meats, bananas, sweet potatoes, sunflower seeds
• Magnesium – supports GABA, relaxes uterus, lowers cortisol
→ Pumpkin seeds, dark leafy greens, dark chocolate, Epsom salt baths
• Selenium – helps detox excess estrogen and support thyroid
→ Brazil nuts (1–2/day), wild fish
• Vitamin E – protects the corpus luteum and supports progesterone synthesis
→ Almonds, sunflower seeds, avocados
4. Reduce estrogen load - give progesterone a chance to function
You may not always have “too much estrogen” — but when progesterone is low, estrogen can feel dominant.
To reduce estrogen overload:
• Support liver detox with cruciferous veggies, dandelion, milk thistle
• Promote daily bowel movements (fiber, magnesium, hydration)
• Try DIM or calcium-D-glucarate (under guidance) for estrogen clearance
• Cut xenoestrogens from plastics, perfumes, and chemical-laden cosmetics
• Avoid synthetic hormones in birth control or hormone-laced meat/dairy
• Castor oil packs over the liver and uterus can reduce stagnation
Also: Incorporate flaxseeds in the follicular phase and sesame + sunflower in luteal phase (seed cycling) to naturally support estrogen and progesterone phases.
5. Consider natural progesterone cream
If you’ve addressed the foundations and still have issues:
• Some women benefit from natural progesterone cream, applied post-ovulation through day 26.
• Avoid using blindly — test and monitor with a practitioner if needed
• Avoid synthetic progestins — they do not activate the same calming and anti-inflammatory receptors
Progesterone cream is used by many with endometriosis with the aim of balancing the estrogen/progesterone hormones. For endometriosis, you may use progesterone cream daily, continuously, or on a cyclic schedule (typically days 12-26 of your cycle), depending on your doctor's advice and the specific product
Note: Not all women tolerate progesterone well.
• If the liver is sluggish, bile is stagnant, or estrogen is dominant, progesterone may convert into unwanted metabolites or trigger side effects (like fatigue, anxiety, or bloating).
• Histamine intolerance, poor methylation, or trauma-induced hormone dysregulation can also interfere with how the body processes progesterone.
• Always support detox and your minerals intake
Optional testing tools
If you want to get precise and know exactly what your hormones are doing:
• DUTCH test – shows progesterone metabolites, cortisol rhythm, and estrogen clearance
• Serum progesterone – test mid-luteal phase (around day 21) to confirm ovulation
• Thyroid panel – include TSH, Free T3, Free T4, and TPO antibodies
It is not a good idea to assume you have high estrogen and testing is always advised. If it is found you have high estrogen then you can use some of the measures mentioned.
Search:
 As featured in:
As featured in:https://pmc.ncbi.nlm.nih.gov/articles
