Treatments for Endometriosis
The various treatments for Endometriosis is an intensely debated subject both in the medical profession and among women who suffer this disease. One of the key problems is that no-one really knows what causes the disease and finding the correct treatment can be hit and miss.
The options for care being offered by conventional modern medicine depends on the severity of the disease, with the main aim being to help alleviate the key symptoms. These being the symptoms of pain and infertility.
There are general points which should be taken into consideration when helping to decide which medical therapy to use.
These options should include:
- The severity of symptoms
- The type of symptoms
- The age of the patient
- The desire to get pregnant or not
- Length of treatment
- Coping with side-effects of drugs
- Cost (in countries where women have to pay for treatment)
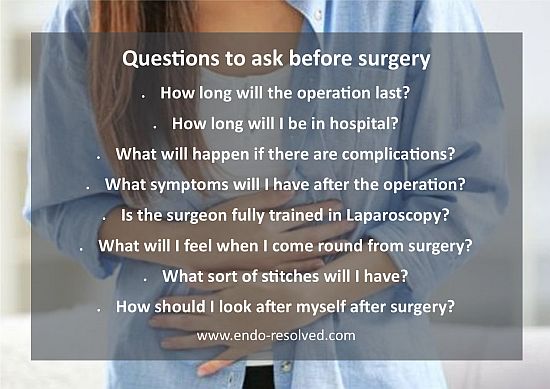
There are various issues you will need to consider before deciding which treatment plan to follow - some of the questions you may have are discussed HERE
How does the treatment work!
The disease is fed by estrogen which is the hormone produced in a woman’s body continuously, but each month there is a surge of this hormone which causes the uterine lining to thicken to prepare for pregnancy.
Then the estrogen levels drop and if there is no fertilisation, the lining of the uterus is shed and a woman has her period. The aim of some drug therapy is to reduce or stop the estrogen being produced in the body, so that it does not continue to feed the disease.
This is achieved by hormone drug therapy. This type of remedy is only successful for milder cases where the growths are relatively small and few in number. In more severe cases then the option of surgery is usually needed to remove the growths.
You may find many different references and names for the growths relating to Endometriosis. They can be called cysts, lesions, endometrial tissue, endometrial cells, as well as implants. These different terms are sometimes used to define different stages of the disease.
Treatment options
The options to manage the disease are usually dependent on the extent or severity of the disease. The options include:
- Observation with no medical intervention
- Hormone medication
- Surgery
- Combined treatment
In detail these include:
Observation with no medical intervention
This approach can be used for milder cases with regular visits to your doctor or gynaecologist to monitor your health. Analgesics may be prescribed to help with any pain, and non-steroidal anti-inflammatory drugs can help.

Hormone Medications
Treatment with hormone drugs can result in temporary improvement of symptoms such as painful periods, pain with intercourse and pelvic pain, but there are many side effects with all drugs offered for the disease.
Drug therapy does not improve the chances for pregnancy, and as it is hormonal based, it will usually delay conception even further due to the hormonal imbalances introduced into the body.
Medication suppresses endometriosis, rather than removing it and is effective only for short term management of symptoms. The active implants returning gradually over 12-24 months after stopping drug management.
The aim of drug therapy is to break the cycle of stimulation and bleeding. By stopping the ovaries usual hormonal cycle and reducing estrogen levels, the endometrial deposits shrink down and become inactive. The disease is still there, and will gradually become reactivated when the normal menstrual cycle starts again.
Ovarian endometriomas of greater than 3 cm diameter are unlikely to respond to medical treatment, and similarly if there are a significant amount of adhesion's - these will respond best to laparoscopic surgery.
Pseudo-pregnancy - a state resembling pregnancy - is used as one method of drug therapy, and this can be achieved through hormone drugs. This approach was developed by observing that endometriosis would regress during pregnancy. Pseudo-pregnancy can be induced by using oral contraceptives containing estrogen and progesterone.
Pseudo-menopause - a state resembling menopause - was developed as another means of managing the disease because it was observed that Endometriosis also regressed after menopause.
Drugs commonly used to treat endometriosis
All of these treatments can have various side effects. Some women suffer more than others, but it is advised to be well informed about them before you decide which to use.
Contraceptive pill - BCP
The contraceptive pill is one of the most commonly used drugs, and is often prescribed for young women with mild disease who also require effective contraception. Despite its long-established use, there has been only one study on the use of the Pill. The study compared the Pill with GnRH agonists and found an equal improvement with both drugs with regards to pelvic pain.
When taking BCP for endometriosis rather than for contraceptive reasons you will take the pills continuously. This means that you will not have a period, as your body thinks that it is pregnant. By doing this you may find you have some spotting as your body adjusts to the pill.
There are some side effects to bear in mind though, and you will need to decide whether the pain of the endometriosis outweighs the risks of taking the pill. Side effects can include weight gain, acne and hair growth on the face. Learn more .....
Gestrinone
Gestrinone is a synthetic hormone that effects the production of oestrogen by the ovaries. It is taken twice weekly rather than daily. Side effects of Gestinone include: weight gain, acne depression, mood swings, hot flushes and loss of libido. Gestrinone is used more commonly in Europe. It works in much the same way as danazol with similar, but milder, side effects.
Danazol
Danazol is a mild form of the male hormone testosterone and reduces the amount of oestrogen produced by the ovaries to around the same level as during menopause.
This is the drug that mimics Pseudo-menopause. Side effects include: weight gain, increased body and facial hair growth, acne, smaller breasts, increased muscle mass, voice deepening and mood swings. Danazol can also cause gasto-intestinal upsets, depression and liver disease.
GnRH agonists
GnRH stands for Gonadotrophin Releasing Hormone, is a drug that acts the same way as the body's own hormone. The body normally makes GnRH in a small gland in the brain (the pituitary) and it is this hormone that stimulates the ovary to develop eggs and produce estrogen, leading to the normal menstrual cycle.
If you take GnRH agonists, this floods the system and confuses the delicately controlled balance, leading to a complete block of egg development, oestrogen production and menstrual cycle. It effectively makes you 'menopausal' for the time that you use the drug, and without the estrogen stimulation, endometriosis shrinks down and becomes inactive.
There are several GnRH analogues available. Examples of GnRH agonists include: goserelin (Zoladex), nafarelin (Synarel), Buserelin (Suprecur) and leuprorelin (Prostap). They are all either given by injection or nasal spray - tablet forms are not available. Side effects of GnHR agonists include: menopausal symptoms such as thinning of the bones, hot flushes, dry vagina, headaches, depression, loss of libido and night sweats.
These side effects can be relieved, by adding back estrogen and progesterone, which does not effect the benefit of treatment. This is known as Add-back therapy. There is now evidence that the use of Add-back hormone replacement therapy (HRT) is effective in preventing the bone thinning and the unpleasant side effects of GnRH treatment.
One of the GnRH drugs which has been commonly prescribed is known as Lupron. There is a lot of information about this drug on the internet, as well as lots of mention of it at forums and social media..
This drug is also used for other health problems in both men and women. So it is not designed specifically for the management of Endometriosis, and some women have found they now have serious long-term health problems caused by this drug.
Progesterone hormone tablets
Progesterone treatment opposes the estrogen effects on the endometrial growths which causes them to ‘shrink’. Progesterone also prevents ovulation which lowers the oestrogen levels. Side effects include: irregular menstrual bleeding, weight gain, mood changes, bloating, fatigue, depression, and nausea. Progestogens are the most commonly used form of medical therapy.
Examples include the drugs medroxyprogesterone acetate (Provera), dydrogesterone and norethisterone. It has long been known that progestogens can alter the blood lipids (fats) in an unfavourable way, which might theoretically lead to an increased risk of blood clots (thrombosis).
Two recent studies have provided more evidence that this could be the case. Although they looked at progestogens used for period problems, the doses used to treat endometriosis are similar, and the risk of thrombosis was found to be around 5-fold higher than expected.
The Mirena Coil
The Mirena Coil is used by some doctors to treat the symptoms of Endometriosis by reducing the amount of blood flow in a woman’s periods.
The Mirena Coil is like many other types of Intrauterine Contraceptive Devices (IUD's or coils) which is fitted by a doctor and remains in the womb for a fixed amount of time. After this time span it must be changed. Most IUD's make a woman's periods heavier, but the Mirena actually makes periods lighter than usual.
Because of this effect, it is frequently used to help deal with heavy periods, and is now used to help with endometriosis, for the reason of reducing blood loss with the menstrual cycle.
It is made of a light, plastic, T-shaped frame with the stem of the 'T' a bit thicker than the rest. This stem contains a tiny storage system of a hormone called Levonorgestrel.
This hormone is also used in contraceptive pills. In the Mirena, however, a much lower dose is released than the Pill (about 1/7th strength), and it goes directly to the lining of the womb, rather than through the blood stream where it may lead to the common progesterone-type side effects.
Although the IUD was originally developed as a contraceptive, the discovery that it leads to much lighter periods was seen as a bonus. Many gynaecologists now suggest the Mirena as a remedy for heavy periods if tablet treatment doesn't work.
Negatives of the Mirena Coil
There are many who feel that the Mirena Coil is very unsuitable as an option to help with the disease, as this particular type of coil increases the risk of developing ovarian cysts.
It is the use of synthetic Progestogen hormones used in the coil that increase this problem. (This is more common with the higher hormone levels associated with the progestogen-only pill.) Overall the risk is about 3 times higher. The device could also lead to other complications of infection in the womb.
Treatment of endometriosis - Part 2 - Surgical Treatment
Reference:
https://en.wikipedia.org/wiki/Endometriosis
https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/treatment
http://endometriosis.org/treatments/